The UK is not alone in dealing with burgeoning waiting lists. Few healthcare systems around the globe have remained unaffected by the COVID-19 pandemic. Once the world returns to a “near normal” will we see a medical tourism boom, driven by pent up demand for surgery?
In many Western developed countries, dealing with the COVID-19 pandemic has become the number one focus and has changed the way that healthcare is delivered. The rapid adoption of teleconsultation and telehealth is clearly here to stay. For many healthcare systems, “beat COVID-19 at any cost” has been the mantra, side-lining healthcare services that patients normally receive either from their public or private healthcare providers.
The UK is an excellent example of this – a country whose national health service for the last year has been dedicated to beating COVID-19 and managing those patients who have been affected by the disease. NHS hospitals have turned operating theatres into ICU spaces, hospital beds have been dedicated to COVID-19 patient care and regular, scheduled acute surgery sessions have been cancelled. The knock-on effect has also impacted the private hospital sector. Private hospital beds, that would usually be occupied by private patients covered either by health insurance or who are self-paying, have been contracted out to the NHS to provide care for acute and urgent, non-COVID-19 NHS patients.
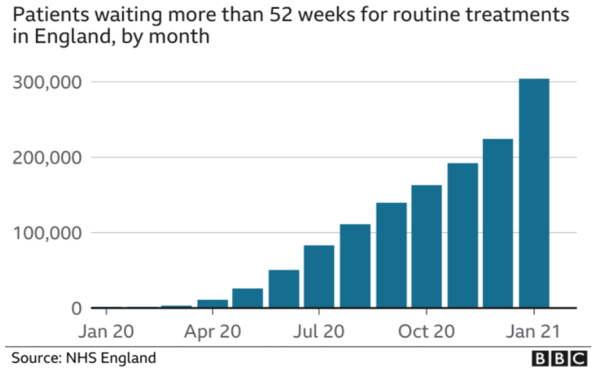
The end result is that if you were a patient waiting for a routine operation under the NHS (a hip or knee replacement, cataract surgery, general surgery etc), you didn’t get treated. The publicly available data on NHS waiting lists demonstrate the massive impact of COVID-19 on the country’s health system. In January 2021, less than half the expected number of routine operations were done, pushing the waiting list to a record high of 4.6m. The number of patients waiting for more than a year for surgery has increased by 100 fold.
Projections by the NHS Confederation suggest that the NHS waiting list is expected to rise from about 4.2 million currently to about 10 million by Christmas 2021. That represents a massive amount of pent-up demand for routine surgery; it will take many years for the NHS to clear the backlog, even if it contracts out large volumes of care to the UK’s private healthcare sector.
It’s a global issue
The UK is not alone in dealing with this issue. Countries across Europe are facing similar challenges. Even where healthcare systems have continued to deliver routine treatment during the COVID-19 pandemic, their theatre capacity has, in effect, been reduced by an estimated 20% due to the constraints imposed by operating in a “Covid-safe” environment. In Germany, hospital rooms with multiple beds have not been able to maximise their occupancy due to physical distancing requirements. Spain and The Netherlands have created lists of procedures that will be prioritised. In some countries with both public and private provision of healthcare (e.g. UK, Italy, Spain), the intention is that increased use of private healthcare providers will offset the overflow of demand in the public system. However, the reality is that a large volume of patients, whether under a public or privately funded healthcare system, are having to wait for non-urgent, non-prioritised surgery. The big question is… will this pent-up demand convert into an upsurge in patients who decide to go abroad for treatment and pay to avoid the wait in their own country?
The patient’s view
Put yourself in the patient’s shoes. You need an operation. It’s not life threatening but it does affect your quality of life. You can live with it, possibly in pain, and it may restrict what you can do from day to day. You know that you will get the operation you need eventually, either funded by your national health system or your health insurer. You have some money set aside “for a rainy day”. You’ll think seriously about using that money to pay for treatment in a private hospital in your own country. That’s a safe bet, if you can afford it. Or will you decide to jump on a plane and travel to a different country with a different culture to get the operation you need at a lower cost and save some of your money for another “rainy day”?
For many people, the decision will be to wait for the funded option to become available within their domestic healthcare system. Some will bear the brunt of the cost for treatment in their local private hospital to get their operation sooner. The relatively small minority will start to consider the options for treatment abroad. They will start looking at costs for surgery in different countries and the travel and accommodation costs for themselves and for a relative or companion. The savings may not add up when they consider the non-treatment related costs, so ruling out this option. They will also consider accessibility – how easy is it to get there (particularly with COVID restrictions on travel) and how safe they feel in travelling for treatment in an unfamiliar health system – ultimately asking, “Do I trust this doctor/hospital/clinic?”. Is the risk worth the reward?
A boom in medical tourism?
I think the honest answer is “Probably not.”
Growth certainly, but not, perhaps, the level of growth that some are hoping for. Most definitely, we will see a significant growth in interest in the medical travel option. Hospitals and clinics will start to receive more enquiries from patients seeking to solve their healthcare issue. Turning that interest into action is the challenge that destinations and providers will face in the post-Covid era. Convincing the patient that medical travel is not only affordable for the patient but that your hospital or clinic can deliver a patient experience that is seamless, worry free, trustworthy and can offer proven success. Perhaps it’s time to audit your communication with enquirers, whether its online, over the phone or by email and ask yourself, “Would I be convinced to do what I’m asking a patient to do?”.








 ©2024 All rights reserved LaingBuisson
©2024 All rights reserved LaingBuisson 


